The knee cap is a large triangular bone that is embedded in a tendon that passes in front of the knee joint. Pain underneath the knee cap or patellofemoral pain syndrome (PFPS) is a common knee complaint in runners. Almost 25% of all new running injuries can due to PFPS. PFPS occurs in women more often than men. Pain usually starts during adolescence when participation in sporting activities is high. Symptoms of PFPS can occur over a prolonged period of time.
If you have PFPS you may experience some of the following symptoms.
- Vague discomfort of the inner knee area, aggravated by activity such s running, jumping, or using stairs.
- You may be more comfortable to sit with your leg straight. The “theater sign” is caused by prolonged sitting with knees in a moderately bent position followed by pain upon arising from a chair.
- A loss of quadriceps (thigh) muscle strength may cause the leg to “give out.” The loss of quadriceps strength can be followed by a reduction in quadriceps muscle mass.
- Mild swelling of the knee area may occur.
 In most chiropody/podiatry offices, the cases of PFPS are usually caused by poor foot posture, however there are a number of factors that can combine together to place stress on your knee cap or patella. These factors include: stability of the footwear; occupation demands; anatomy around the knee joint; intensity of training if you are a runner or walker; and foot instability. The preferred treatment approach is non-surgical. You are advised to rest during periods of pain and refrainfrom pain provoking activities.
In most chiropody/podiatry offices, the cases of PFPS are usually caused by poor foot posture, however there are a number of factors that can combine together to place stress on your knee cap or patella. These factors include: stability of the footwear; occupation demands; anatomy around the knee joint; intensity of training if you are a runner or walker; and foot instability. The preferred treatment approach is non-surgical. You are advised to rest during periods of pain and refrainfrom pain provoking activities.
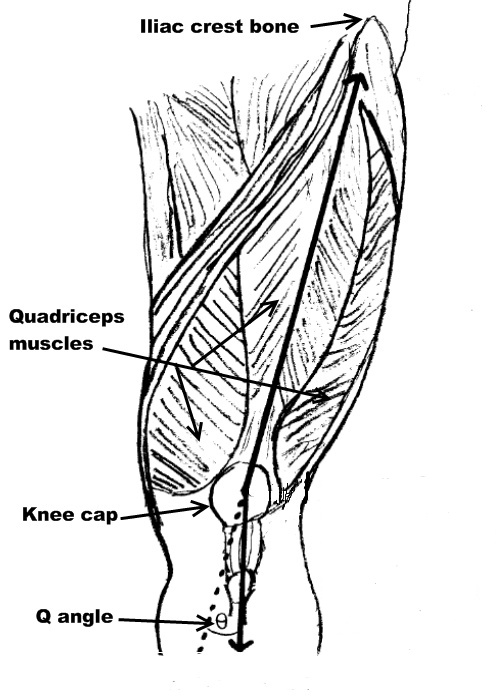
To make sense of this injury, you need a basic understanding of the anatomy in the front of the knee. The quadriceps muscle originates in the pelvis above the hip joint and continues toward the knee joint where it attaches to the patella. The patellar ligament continues from below the patella and attaches into the tibia below the knee joint. The quadriceps keeps your knee joint straight when you stand, but more importantly, the quadriceps keeps the knee stable as the knee bends. The quadriceps is a grouping of 4 muscles. The patella acts like a pulley as the knee bends causing the patella to be pressed in to a groove in the femur. If all of the 4 quadriceps muscles are balanced, the patella will move within the femoral groove without any causing any pain.
Causes of patellofemoral syndrome
- Weakness of one of the quadriceps muscles called the vastus medialis. If the muscle is weak it will cause the patella to displace out of the femoral groove.
- Tightness of the muscles around the knee.
- Tightness of the soft tissues that keep the patella in the femoral groove.
- The patella can be displaced from the femoral groove due to a large Q angle. Females have a wider pelvis resulting in a larger Q angle when compared to males. The Q angle is formed from the intersection of two lines through the patella. The first line is drawn from a point in the front of the hip bone called the iliac crest to the middle of the patella. The second line is from the middle of the patella to a bony tubercle on the tibia. Displacement of the patella results in less surface between the patella and the femur. This causes an increase in pressure underneath the knee cap resulting in pain.
- The Q angle can increase if the foot is excessively pronated. The Q angle can be measured while lying down and standing. A custom foot orthotic is indicated if there is an increase in the Q angle from lying to standing.
- Increased intensity of activity
Chiropodists and podiatrists will evaluate if a pronated foot is having an impact on the Q angle, however, a referral to a physiotherapist, sports medicine physician or orthopedic surgeon maybe required if other causes of patellofemoral syndrome are identified.
The treatment strategies for PFPS include:
- Rest from activity
- Icing
- Oral anti inflammatories
- Physical therapy modialities
- Muscle training
- Stretching of muscles around knee
- Massage
- Knee bracing and taping
- Custom foot orthotics and stability footwear
